주메뉴
- About IBS 연구원소개
-
Research Centers
연구단소개
- Research Outcomes
- Mathematics
- Physics
- Center for Theoretical Physics of the Universe(Particle Theory and Cosmology Group)
- Center for Theoretical Physics of the Universe(Cosmology, Gravity and Astroparticle Physics Group)
- Center for Exotic Nuclear Studies
- Center for Artificial Low Dimensional Electronic Systems
- Center for Underground Physics
- Center for Axion and Precision Physics Research
- Center for Theoretical Physics of Complex Systems
- Center for Quantum Nanoscience
- Center for Van der Waals Quantum Solids
- Chemistry
- Life Sciences
- Earth Science
- Interdisciplinary
- Institutes
- Korea Virus Research Institute
- News Center 뉴스 센터
- Career 인재초빙
- Living in Korea IBS School-UST
- IBS School 윤리경영


주메뉴
- About IBS
-
Research Centers
- Research Outcomes
- Mathematics
- Physics
- Center for Theoretical Physics of the Universe(Particle Theory and Cosmology Group)
- Center for Theoretical Physics of the Universe(Cosmology, Gravity and Astroparticle Physics Group)
- Center for Exotic Nuclear Studies
- Center for Artificial Low Dimensional Electronic Systems
- Center for Underground Physics
- Center for Axion and Precision Physics Research
- Center for Theoretical Physics of Complex Systems
- Center for Quantum Nanoscience
- Center for Van der Waals Quantum Solids
- Chemistry
- Life Sciences
- Earth Science
- Interdisciplinary
- Institutes
- Korea Virus Research Institute
- News Center
- Career
- Living in Korea
- IBS School
News Center
| Title | Regulating the Immune System's 'Regulator' | ||
|---|---|---|---|
| Embargo date | 2018-11-20 12:00 | Hits | 1381 |
| Press release | |||
| att. | |||
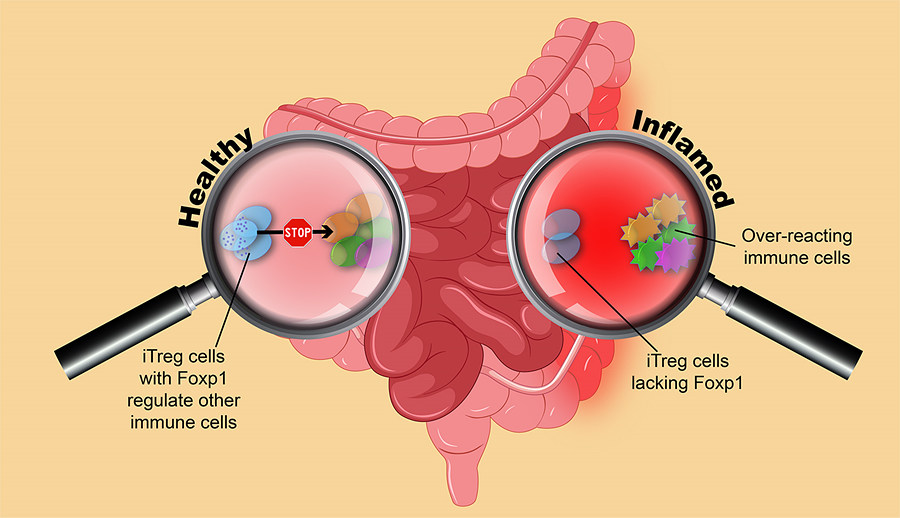
Regulating the Immune System's 'Regulator'- Immune cells that curb over-reacting immune responses need Foxp1 protein - A research team at the Academy of Immunology and Microbiology, within the Institute for Basic Science (IBS) has discovered a possible therapeutic target that pulls the reins of immunity. On Nature Communications, the scientists reported that mice lacking Foxp1 protein in some specific immune cells are more susceptible to immune-induced inflammation. The immune system is capable of protecting the body from invading pathogens, but it can also over-react and cause allergies and autoimmunity. In this respect, regulatory T (Treg) cells are an important built-in "self-check" of the immune system: they put a break to other cells, preventing excessive immune reactions from happening. Since their discovery, Treg cells have been studied extensively as compelling and multifaceted therapeutic supplement. For example, Treg cells could be valuable to block the unruly immune responses in autoimmune diseases, like Crohn's disease or inflammatory bowel disease. Vice versa, in the case of tumors, Treg cells would need to be restrained to let anti-tumor immune response act more freely. In the past decade, it has been established that broadly speaking, two different types of Treg cells exist in mammals: thymic Treg (tTreg) and induced Treg (iTreg). tTreg cells are generated at a neonatal age in the thymus, and protect us from fatal autoimmune reactions. Whereas iTreg cells form later in life and accumulate predominantly at mucosal barriers, such as: intestine, lungs, etc. In the large intestine, iTreg cells are essential to prevent an overenthusiastic immune response to fight against useful gut bacteria and harmless food. iTreg cells could be good candidates for therapeutic interventions. iTreg precursors, unlike tTreg cells, could potentially be isolated from the host, modified, expanded in the laboratory, and subsequently transferred back to the host. Researchers are, however, facing problems with iTreg's stability: once generated, these cells tend to lose their regulatory identity and convert to other cell types. "It is necessary to find out molecules that control the fate of iTreg cells," says IBS researcher and the first author of the study, Sayantani Ghosh. In this study, IBS researchers found that Foxp1 provides stability to iTreg cells, by interacting with the gene encoding its "sibling": Foxp3 – the protein that confers identity to Treg cells. iTreg cells lacking Foxp1 gradually lose Foxp3, and become unable to perform their regulatory functions against excessive immunity. In mice, the lack of Foxp1 in iTreg cells led to intestinal inflammation and increased susceptibility to colitis. Moreover, IBS biologists showed that Foxp1 is essential for sustaining optimal expression of Foxp3 specifically in iTreg cells, not in tTreg cells. "In a venture to spot differences hidden behind cells with similar appearances, we found Foxp1. The results suggest that this protein could be used to engineer more stable iTreg cells, while keeping their thymic counterparts untouched," explains Dipayan Rudra, corresponding author of the study.
Dipayan Rudra and Letizia Diamante Notes for editors - References - Media Contact - About the Institute for Basic Science (IBS) |
|||
|
|
|||
| Next | |
|---|---|
| before |
- Content Manager
- Communications Team : Kwon Ye Seul 042-878-8237
- Last Update 2023-11-28 14:20